Management of Lymphoma in a Domestic
Rat (Rattus norvegicus)
Susan Harris (veterinary student)a
Heather Wilson, DVM, DABVP (Avian)b
Michelle Wall, DVM, DACVIMc
Jamie McGill (veterinary student)a
Tracy Geiger, DVM, DACVIMb
aUniversity of Georgia College of Veterinary Medicine Athens, Georgia
bDepartment of Small Animal Medicine University of Georgia College of Veterinary Medicine Athens, Georgia
cUpstate Veterinary Specialists Greenville, South Carolina
Materials and Methods
A 2½-year-old, 432-g male neutered rat (Rattus norvegicus) was evaluated for intermittent bilateral hindlimb lameness. Physical examination revealed porphyrin epiphora of the left eye. All other physical examination findings were within normal limits. No obvious crepitus was evident in the joints of the pelvic limb, and no lesions associated with the hindlimbs were noted. On palpation, no obvious pain was observed in the vertebral column or pelvic limbs. The rat was treated with meloxicam 0.2 mg/kg PO q24h (Metacam, 1.5 mg/mL oral suspension, Boehringer Ingelheim Vetmedica) for possible degenerative joint disease.
One month later, the rat developed hematuria and bilateral proprioceptive deficits in the pelvic limbs. The rat was alert and responsive, and auscultation of the heart and lungs was normal. Physical examination abnormalities included enophthalmia, blepharospasm, and chronic porphyrin epiphora of the left eye; left popliteal lymph node enlargement; and paresis in the rear limbs with bilateral scuffing of the dorsal surface of the pelvic feet on ambulation. Withdrawal reflexes were normal in both hindlimbs. Examination of the thoracic limbs and cranial nerve evaluation were unremarkable. There was no evidence of muscle atrophy or pain on palpation of the vertebral column or pelvic limbs.
Initial diagnostic evaluation included a urinalysis of a voided sample, hematology, plasma biochemistry profile, and thoracic and abdominal radiographs. Abnormalities detected on the urinalysis included large amounts of blood, a pH of 6, and proteinuria (2+). Gram-negative rods were noted on cytologic examination of the sediment. Hematology revealed mild, regenerative anemia (34%, with 2.3+ polychromasia; reference range, 37%.49%*), mild leukocytosis (13.1 × 10³/µL; reference range, 4.10.2 × 10³/µL) characterized by neutrophilia (5.24 × 10³/µL; reference range, 0.24.1.734 × 10³/µL), lymphocytosis (6.812 × 10³/µL; reference range, 0.36.3.468 × 10³/µL), monocytosis (0.786 × 10³/µL; reference range, 0.0.51 × 10³/µL), and eosinophilia (0.262 × 10³/µL; reference range, 0.0.612 × 10³/µL). Biochemical abnormalities included hyperglycemia (182 mg/dL; reference range, 74.163 mg/dL), hypokalemia (3.5 mmol/L; reference range, 4.3-6.3 mmol/L), and hypomagnesemia (1.7 mg/dL; reference range, 2.6-3.2 mg/dL).
 Figure 1. Right lateral thoracic radiograph of a domestic rat demonstrating a soft tissue opacity within the thorax that silhouetted the heart and caused dorsal displacement of the trachea. |
 Figure 2. Right lateral thoracic radiograph of the same patient 6 months previously demonstrating a normal chest. |
The patient was anesthetized by masking down with isoflurane in oxygen using a nonrebreathing circuit. Right lateral thoracic radiographs revealed increased soft tissue opacity within the thorax that silhouetted the heart and caused dorsal displacement of the trachea (Figure 1). This mass had not been evident on radiographs taken 6 months previously as part of the patient’s diagnostic workup for respiratory disease (Figure 2). Abdominal radiographs revealed increased osteophyte production evident in both stifle joints, consistent with degenerative joint disease and vertebral spondylosis in the lumbar spine. Enrofloxacin 10 mg/kg PO q12h for 10 days (Baytril, 68-mg tablets [Bayer Animal Health] compounded in a 20-mg/mL suspension at the University of Georgia Veterinary Teaching Hospital) was prescribed for treatment of the urinary tract infection. Meloxicam was continued at 0.2 mg/kg PO q24h.
Reexamination 10 days after initial presentation indicated resolution of the hematuria and decreased porphyrin tearing. A weight loss of 9 g, tachycardia of 340 bpm, and tachypnea of 120 breaths/min were noted. Evaluation of the hindlimbs revealed delayed proprioception, absent postural thrust, severely decreased hopping in the right hindlimb, and mildly decreased hopping in the left hindlimb. The left popliteal lymph node remained enlarged.
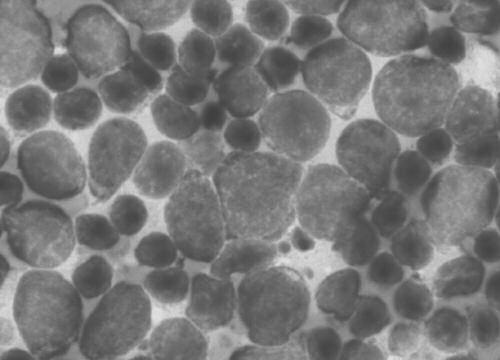
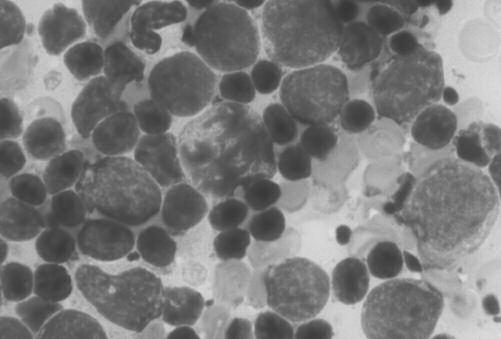
Repeat urinalysis failed to indicate any evidence of bacterial infection. The patient was anesthetized as previously described, and thoracic ultrasonography revealed a 2.5 × 3-cm mass within the cranial mediastinal region. An ultrasound-guided aspirate of the mass revealed diffuse small, well-differentiated lymphocytes and large lymphoblasts, with mitotic figures frequently observed (Figure 3). The aspirate was consistent with a diagnosis of lymphoma.
|
|
|
| Figure 3. (A and B) Aspirate samples from the mediastinal lymph node revealing diffuse lymphocytes. | ||
Initial therapy for lymphoma consisted of L-asparaginase 400 IU/kg SC (Elspar, 5,000 IU/mL, Merck), lomustine 1-mg capsule PO (CeeNU, Bristol Laboratories, Princeton, NJ), and prednisone 1.6 mg/kg PO q24h (Pediapred, 1-mg/mL syrup, Roxane Laboratories, Columbus, OH) (Table 1). Because of the difficulties in giving a lomustine capsule orally to a rat, the capsule was broken apart while the veterinarian was wearing double masks and rubber gloves, and its contents were mixed in a palatable liquid at each dosing. Any remaining drug and the capsule, masks, gloves, and syringe were discarded following a proper chemotherapy disposal protocol.
Although the rat initially appeared to respond to chemotherapy as evidenced by an initial weight gain of 5 g over 10 days and increased activity level, it was euthanized 66 days after the onset of therapy because of acute progressive dyspnea.
Discussion
Based on cytologic findings, the provisional diagnosis was mediastinal lymphoma. A clinical pathologist did confirm this diagnosis; however, it was not confirmed at necropsy.
Lymphoma is a proliferative cancer originating in lymphoid tissues involving any organ or tissue.1,2 Mediastinal lymphoma, which most commonly involves the anterior and posterior lymph nodes in the mediastinum, is generally associated with a poor prognosis.1 Clinical signs vary with the location and extent of the disease.1 Clinical signs of the mediastinal form include dyspnea, tachypnea, and uncompressible anterior mediastinum with dull heart and lung sounds.1
Chemotherapy has played a role in cancer management for many years.3 Chemotherapeutic agents used in combination have a greater advantage over the use of a single chemotherapeutic agent.3,4 Combination therapy allows maximal killing of cells while maintaining an acceptable toxicity range, the expansion of the therapeutic range against the tumor cells, and the prevention or slowing of the development of resistant cells.5 In this case, the rat was treated with a combination of L-asparaginase and lomustine, along with daily prednisone. L-asparaginase is a bacteria-derived enzyme that degrades the amino acid asparagine, deprives growing cells of asparagine, and causes an inhibition of protein synthesis. It is used in combination with other chemotherapeutic drugs for the treatment of lymphoma.6 Tumor cells may become resistant to the antitumor effects of L-asparaginase, and allergic reactions can develop following repeated administration because of the production of antibodies against the protein components of the drug.6 Lomustine is an alkylating chemotherapeutic agent used to treat resistant lymphoma in dogs.6 Primary side effects include myelosuppression and hepatotoxicity.4,6 Prednisone also has antitumor activity against lymphoma.6
Because cachexia is one of the most common paraneoplastic syndromes seen in veterinary cancer patients, it is important to begin nutritional supplementation early in the patient’s treatment.7 It is often necessary to use a high-calorie, high-protein supplement as an adjunct therapy in cases of lymphoma.8 In this case, the rat received 3 to 5 mL a day of Ensure (Abbott Laboratories), along with various types of baby food to help it maintain weight and for easy delivery of daily medication.
Table 1. Chemotherapy Protocol Used in a Domestic Rat with Lymphoma |
||
|---|---|---|
| Week | Drug | Dose |
| 1 | L-asparaginase Prednisone Diphenhydramine (pre-med) |
400 IU/kg SC 1.6 mg/kg PO q24h 2 mg/kg PO |
| 2 | Lomustine Prednisone |
1 mg PO 1.6 mg/kg PO q24h |
| 3 | L-asparaginase Prednisone Diphenhydramine (pre-med) |
400 IU/kg SC 1.6 mg/kg PO q24h 2 mg/kg PO |
| 4 | Prednisone | 1.6 mg/kg PO q24h |
| 5 | Lomustine Prednisone |
1 mg PO 1.6 mg/kg PO q24h |
| 6 | Prednisone | 1.6 mg/kg PO q24h |
| 7 | Prednisone | 1.6 mg/kg PO q24h |
| 8 | Lomustine Prednisone |
1 mg PO 1.6 mg/kg PO q24h |
| 9 | Prednisone | 1.6 mg/kg PO q24h |
| 10 | Prednisone | 1.6 mg/kg PO q24h |
Conclusion
With little information in the literature on the use of chemotherapeutic agents and the prognosis of cancers in exotic animals, the goal for this patient was to control the cancer and prolong survival while still maintaining a good quality of life.5 The chemotherapy was not designed as a cure for the patient’s lymphoma but as a palliative therapy. While undergoing treatment, the rat maintained a good quality of life, and it is believed that the rat’s life was extended by approximately 2 months. This is approximately one-tenth the total life span of a rat (with an average life span of 2 years). This is relatively comparable to the median remission time of 12 months in a dog (with an average life span of 10 years) being treated for lymphoma with chemotherapy.9
*All reference ranges are taken from Williams BH, Weiss CA: Section four: Small rodents, basic anatomy, physiology, husbandry, and clinical techniques, in Quesenberry KE, Carpenter JW (eds): Ferrets, Rabbits, and Rodents: Clinical Medicine and Surgery, ed 2. Philadelphia, WB Saunders, 2004, pp 290-291.
References
- Vail DM, MacEwen EG: Hematopoietic tumors, feline lymphoma and leukemias, in MacEwen EG, Withrow SJ (eds): Small Animal Clinical Oncology, ed 3. Philadelphia, WB Saunders, 2001, pp 590, 592-593, 597, 606.
- de Gopegui RR, Feldman BF: Lymphatic diseases, in Leib MS, Monroe WE (eds): Practical Small Animal Internal Medicine. Philadelphia, WB Saunders, 1997, pp 964-967.
- Rosenthal RC: Chemotherapy, in Feldman EC, Ettinger SJ (eds): Textbook of Veterinary Internal Medicine: Diseases of the Dog and Cat, ed 4. Philadelphia, WB Saunders, 1995, pp 473-482.
- Couto CG: Part II: Oncology, principles of cancer treatment, practical chemotherapy, in Couto CG, Nelson RW (eds): Small Animal Internal Medicine, ed 3. St. Louis, Mosby, 2003, pp 1100-1131.
- Kent MS: The use of chemotherapy in exotic animals. Vet Clin North Am Exotic Anim Pract 7(3):807-820, 2004.
- Chun R, Garrett L, MacEwen EG: Cancer chemotherapy, in MacEwen EG, Withrow SJ (eds): Small Animal Clinical Oncology, ed 3. Philadelphia, WB Saunders, 2001, pp 97, 104, 107-108.
- Grahm JE, Kent MS, Théron A: Current therapies in exotic animal oncology. Vet Clin North Am Exotic Anim Pract 7(3):757-781, 2004.
- Williams BH, Weiss CA: Section one: Ferrets, neoplasia, in Quesenberry KE, Carpenter JW (eds): Ferrets, Rabbits, and Rodents: Clinical Medicine and Surgery, ed 2. Philadelphia, WB Saunders, 2004, pp 97-100.
- Vail DM, MacEwen EG, Young KM: Hematopoietic tumors, canine lymphoma and lymphoid leukemias, in MacEwen EG, Withrow SJ (eds): Small Animal Clinical Oncology, ed 3. Philadephia, WB Saunders, 2001, pp 560-561, 570-574.
This Case Report is reposted from AEMV Journal of Exotic Mammal Medicine and Surgery, 3(2), 1-4 (December 2005) with permission of the authors. It has been reformatted to accommodate mobile screens, but contains the same information as the original.


